United Health Care (AARP) announced today they were waiving the cost share on Medicare Advantage plans. The following is the announcement:
Member’s health is our priority. Recently, we shared news that UnitedHealth Group is taking additional action to directly support people affected by the COVID-19 pandemic by providing over $1.5 billion of additional support for our customers. We wanted to share more details with you.
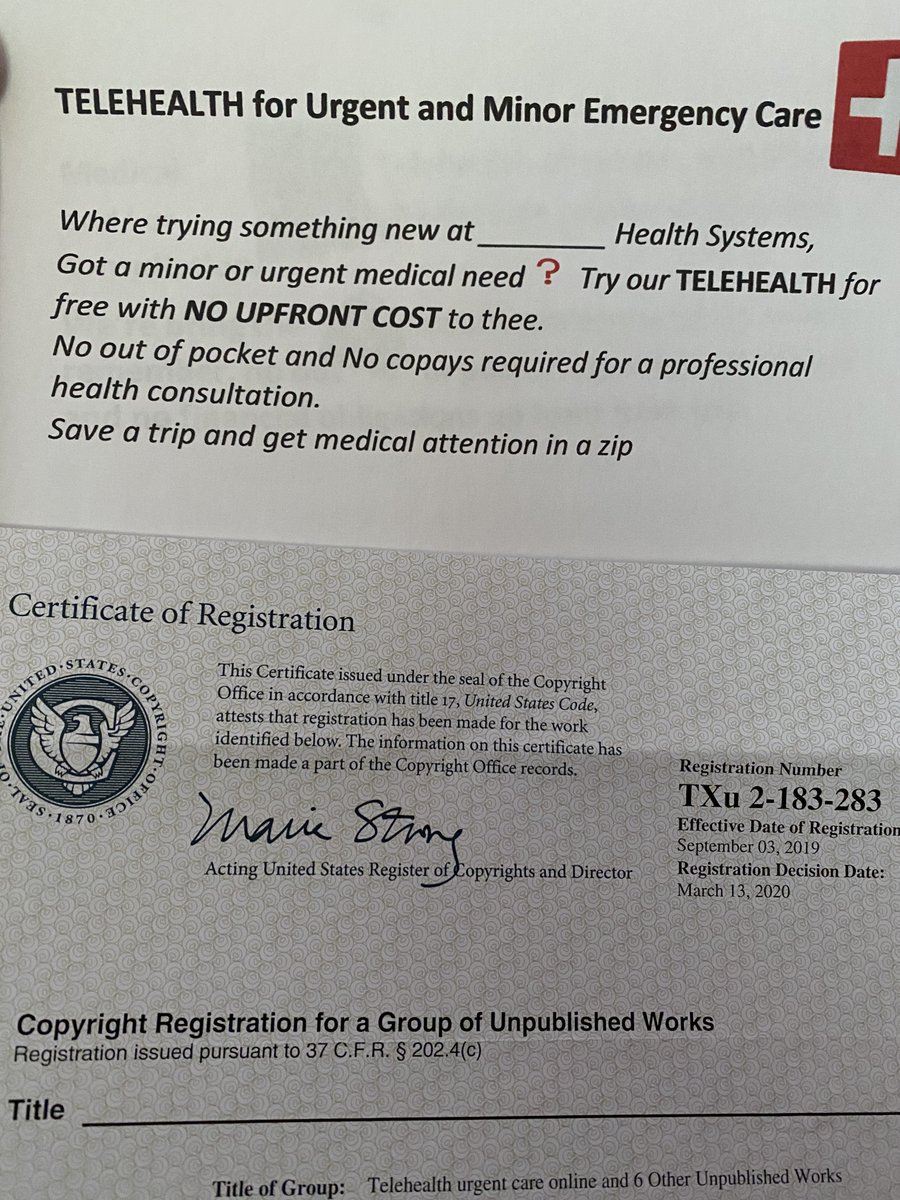
To help member’s get the care they need, we are waiving cost-share (copays, coinsurance and deductibles) for our Medicare Advantage plan members as follows. Members will have a $0 copay for primary care provider (PCP) and specialist physician services, as well as other covered services (listed below) between May 11, 2020 until at least September 30, 2020. By lowering our PCP and specialist copays to $0, along with our telehealth cost-share waiver, we hope to help make it easier for member’s to access care.
Members will have no copays, deductibles or coinsurance for covered COVID-19 testing and related services; this includes laboratory testing, specimen collection and certain related services that result in the ordering or administration of the test, including physician office or emergency department visits. To choose the best dental insurance plans with no waiting periods, we primarily looked at several factors related to cost, such as monthly premiums, copays or coinsurance rates, annual limits,.
Services included
The following services, if covered by a member’s plan, are eligible for a $0 copay under the cost share waiver, but do not include diagnostic tests and certain other services.
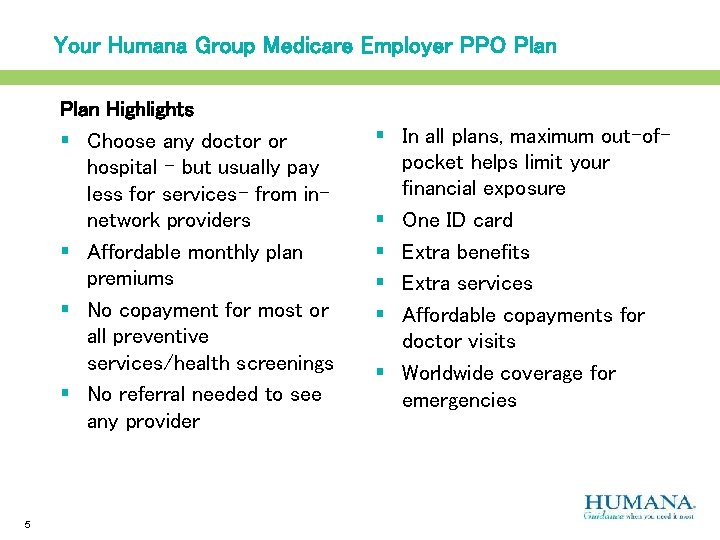
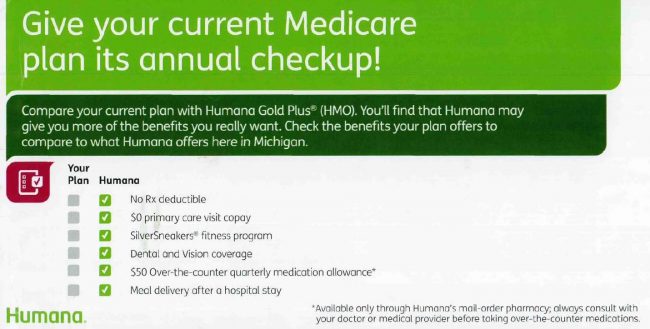
No Copay For Humana

- Primary care provider (PCP) office visits
- Specialist physician office visits
- Physician assistant or nurse practitioner office visits
- Medicare-covered chiropractic and acupuncture services
- Podiatry services and routine eye and hearing exams
- Physical therapy, occupational therapy and speech therapy
- Cardiac and pulmonary rehabilitation services
- Outpatient mental health and substance abuse visits
- Opioid treatment services
Humana Health Insurance No Copay
The $0 copay applies to services from a network provider and out-of-network services covered by the plan.
Member cost share is not waived for the following services, unless they are related to COVID-19 testing or treatments:

- Lab and Diagnostic tests (radiological and non-radiological)
- Part B and Part D drugs
- Durable Medical Equipment, Prosthetics, Orthotics and Supplies
- Renal Dialysis
- Other services not covered by your plan
Copays, Coinsurance and deductibles for services in the following settings are not waived. Members will be responsible for their share of the cost under their benefit:
- Inpatient hospital and Outpatient surgery or observation services
- Skilled Nursing Facilities
- Emergency, Urgent and Ambulance services
Eligible Members
The cost-share waiver applies to all UnitedHealthcare Medicare Advantage members, including members of Special Needs Plans (SNP) and UnitedHealthcare Group Medicare Advantage plans.
Humana Copay Schedule
This information is posted on our UnitedHealthcare COVID-19 Health and Wellness page for members. Thank you for being a partner in care to our members during this time.
